Pilates at The Rehab Hub
Book Clinic








TESTIMONIALS
Why Stagnant Bodies Die Like Stagnant Water
Think about water for a moment.
A flowing stream teems with life. Fish swim, plants grow, oxygen circulates. Everything thrives.
But stagnant water? It's a graveyard. No oxygen. No life. Just decay.
I see the same thing happening in rehabilitation every day. Patients restricted from movement, told to rest, to avoid activity. Their bodies become like stagnant ponds.
Then something magical happens when they start moving again. You start to feel as though they're alive.
The Real Problem: Fear of Movement
The biggest barrier to recovery isn't what clinicians think—it's what patients fear.
Most patients come to us terrified of movement. They've been hurt. They've been told to rest. They've learned to associate movement with pain, with danger, with making things worse.
This fear makes perfect sense. When something hurts, our brain's protective instinct screams "stop" to prevent further damage. But here's the tragedy: that same protective instinct often becomes the very thing that prevents recovery.
The real flaw isn't in our clinical understanding—it's that most practices aren't equipped to address this fear. We're not set up to teach patients how to move fearlessly, how to distinguish between protective pain and healing discomfort.
The brain's ability to adapt and change occurs through neuroplasticity. This mechanism allows damaged brains to relearn lost behaviors in response to rehabilitation.
Without movement, this process stalls. The brain stays stuck in its damaged state.
Movement as Actual Medicine
I've watched patients transform when we shift from seeing movement as something they "should do" to recognising it as medicine they desperately need.
The science backs this up completely. Exercise-induced neuroplasticity changes serve as key rehabilitation treatment mechanisms. Brain-derived neurotrophic factor (BDNF) acts as a crucial protein in neuroplasticity events after exercise.
This isn't just theory. Physiotherapy treatment produces measurable increases in parasympathetic nervous system activation and decreases in subjective pain perception.
When patients understand this—when we can help them overcome their fear of movement—everything changes. They stop seeing movement as dangerous and start seeing stillness as the real threat.
The Nervous System Reset
The transformation happens when we teach patients to move without fear. We focus on building and calming the nervous system simultaneously, helping them distinguish between protective responses and actual danger.
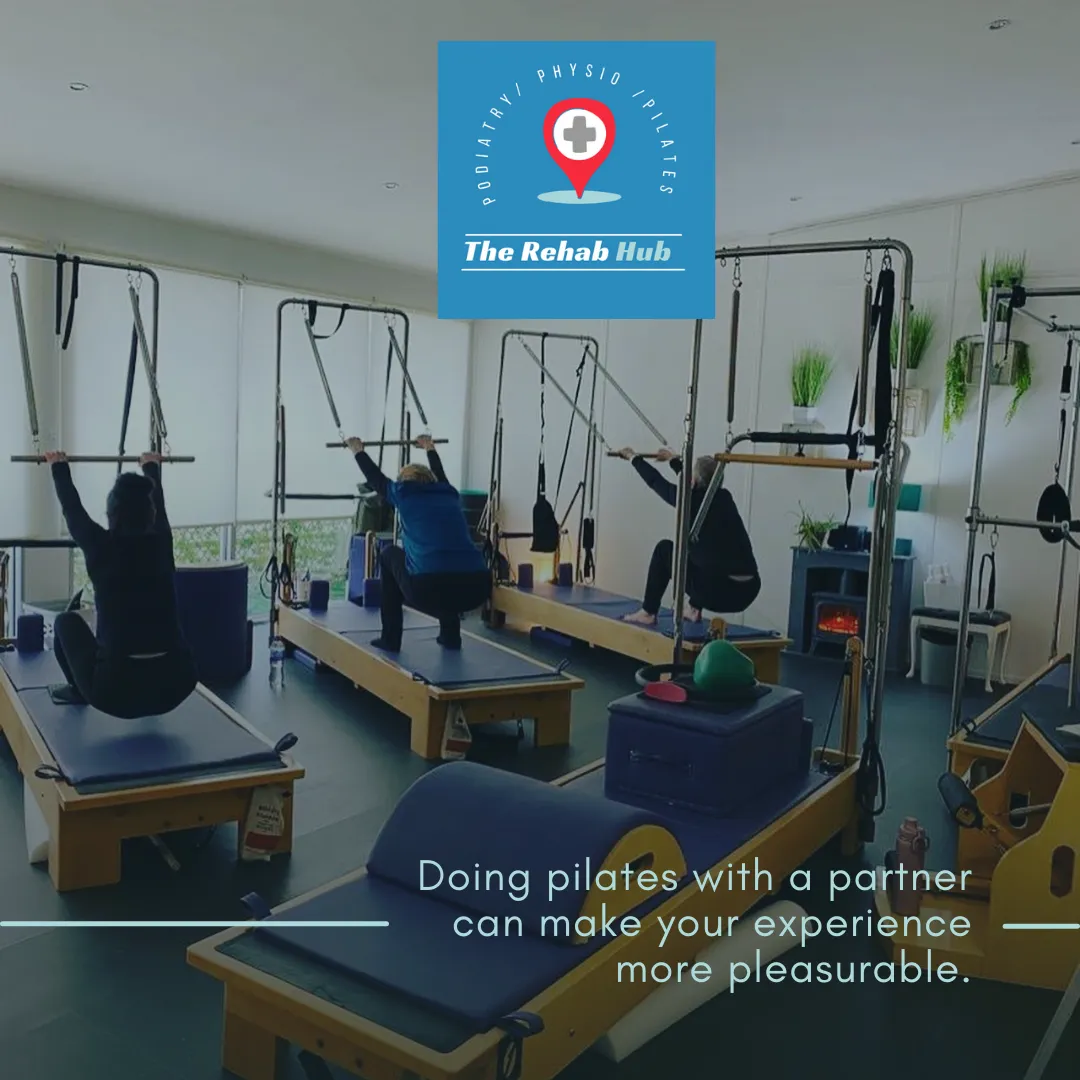
Through breath work, mindful movement, and parasympathetic activation, patients learn to regulate their internal state. This is why we use the Pilates method in our clinical practice.
Clinical Pilates combines traditional principles like centering, concentration, and breath awareness with neurological rehabilitation principles. It's movement as medicine in its purest form.
Through this approach, patients learn to move mindfully and fearlessly. They discover they can influence their pain, their anxiety, their recovery through intentional movement and breathing. Most importantly, they learn that movement won't hurt them—it will heal them.
Breaking Down the Silos
Traditional rehabilitation keeps everything separate. Physical therapy here. Mental health there. Medical interventions somewhere else.
But bodies don't work in silos. Neither should rehabilitation.
Integrated treatment teams minimise invalidation and hold together mind and body. This integration gets embedded within the treatment approach itself.
When we assemble truly integrated care, we can deliver highly individualized treatment that simultaneously addresses brain, body, and mind.
The results speak for themselves. Patients experience higher bodily awareness, greater mental health, and increased social interaction. Their happiness and quality of life improve dramatically.
The Clinical Reality
In practice, this means rethinking everything about how we approach rehabilitation.
Instead of restricting movement, we teach patients to embrace it fearlessly. Instead of separating disciplines, we integrate them. Instead of just treating symptoms, we address the fear that keeps patients stuck.
Most practices aren't equipped for this. They lack the tools, the training, the mindset to help patients overcome their deep-seated fear of movement. This is where the real transformation needs to happen.
Every session becomes an opportunity to activate the parasympathetic nervous system. Every movement becomes a chance to rewire neural pathways. Every breath becomes medicine.
Our job is to teach patients to recognise the difference between protective pain and healing discomfort. We help them develop the confidence to move through fear, to trust their bodies again, to see movement as their ally rather than their enemy.
The Future of Rehabilitation
We're moving toward a future where movement gets recognised as fundamental medicine. Where integration becomes the standard, not the exception.
This matters more than most people realize. Globally, one in three people live with health conditions that benefit from rehabilitation. With aging populations and increasing chronic disease, rehabilitation has become a priority health strategy for the 21st century.
The old model of compartmentalised, reactive treatment is dying. The future belongs to preventative, holistic approaches that address the interconnected nature of physical, psychological, and social well-being.
Patients become active participants in their recovery rather than passive recipients of care. They learn to see their bodies as dynamic systems capable of healing and adaptation.
From Stagnation to Flow
The water metaphor holds true throughout rehabilitation. Stagnation leads to death. Movement creates life.
When we help patients transition from stagnant to flowing, we witness something profound. They don't just recover. They come alive.
Their nervous systems regulate. Their pain decreases. Their confidence returns. Their bodies remember how to heal.
This is what rehabilitation looks like when we finally understand that movement isn't just helpful. It's medicine.
And like all medicine, it works best when prescribed intentionally, administered skillfully, and integrated into a comprehensive treatment approach.
The future of rehabilitation isn't about choosing between movement and rest, between physical and mental health, between disciplines and approaches.
It's about integration. It's about flow. It's about recognising that in both water and bodies, movement is what keeps everything alive.
Address and Email
Email: [email protected]
Address
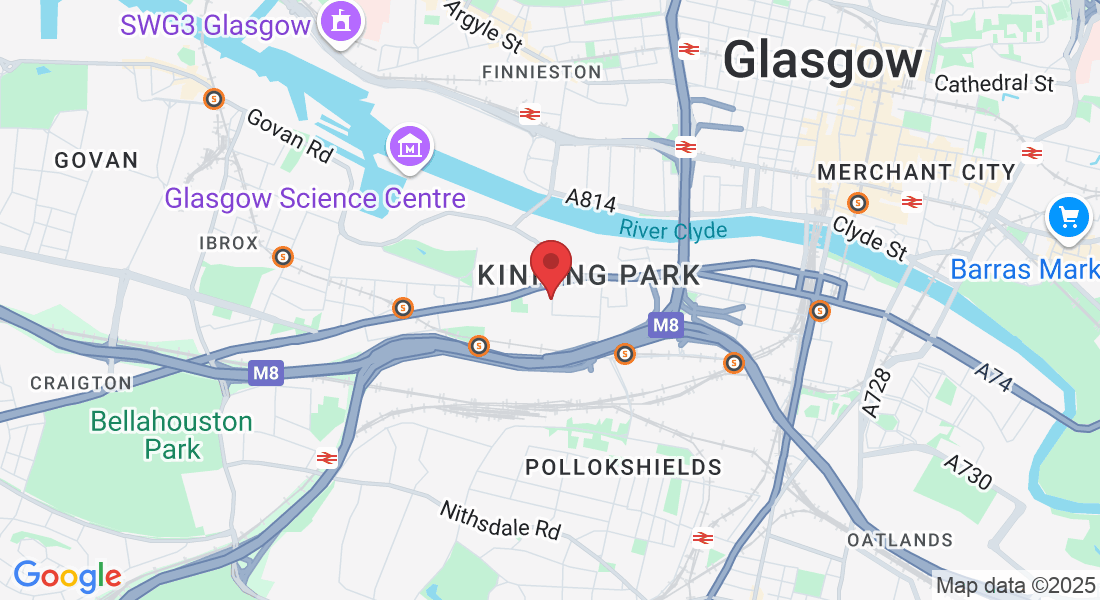
Kinning Park Clinic:
Clinic: 32 Portman Street, Glasgow, G41 1EJ
The Rehab Hub is conveniently located at three prime locations in Glasgow. Two of our locations offer Reformer Pilates.
Kinning Park Studio: Situated at 32 Portman Street, Glasgow, G41 1EJ, this studio offers ample free on-street parking. It's close to Shields Road and Kinning Park underground stations and is easily accessible from the M8, M77, and M74 motorways. Numerous bus routes on Paisley Road West make our studio highly accessible. Check out our video guide to see our studio and learn more:
reformerglasgow.co.uk/kinningpark
Get In Touch
Assistance Hours
Mon – Thursday 9:00am – 8:00pm
Friday 9:00am - 3:00pm
Saturday 9:00am - 2:00pm
Sunday – 9:00am - 1.:00pm
Phone Number:
0141 363 0306
Address and Email
Email: [email protected]
Address
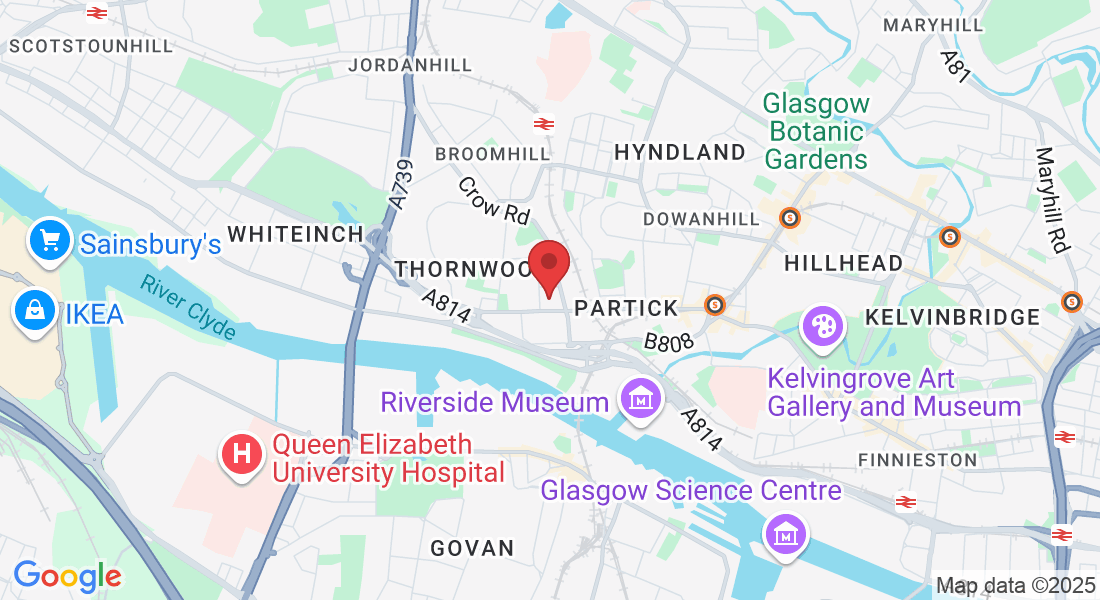
West End Clinic:
Unit 1, 31 Crow Road, Partick, G11 7RT
Partick Studio: Located at Unit 1, 31 Crow Road, Partick, Glasgow, G11 7RT, our Partick studio is easily reachable via public transportation, with the Partick train and subway stations nearby. There are multiple bus routes along Dumbarton Road that stop close to the studio. Additionally, there is 2 hours of free parking available in the West End Retail Park right next to the studio, as well as ample on-street parking. We’re located just off Crow Road, across from the big Marks & Spencer at the retail park.
Look for the sign that says "Freelance Windows" — we’re right in the lane next to it.
Video Link of location to West End:
Get In Touch
Assistance Hours
Mon – Thursday 9:00am – 8:00pm
Friday 9:00am - 3:00pm
Saturday 9:00am - 2:00pm
Sunday – 9:00am - 1.:00pm
Phone Number:
0141 363 0306